对于激素受体(HR)阳性的晚期乳腺癌(ABC),当前的内分泌治疗疗效有了显著的提高,在一线内分泌治疗的试验中,可观察到无进展生存时间(PFS)获得了一致的提高。在2016年圣安东尼奥乳腺癌大会上,来自巴西的学者报告了一项文献系统回顾,评估了芳香化酶抑制剂(AI)一线单药治疗HR+ABC所取得的PFS的时间演变。
在这项文献回顾中,研究者检索了内分泌治疗HR+ABC的随机临床试验,选择了2000年之后涉及AI单药一线治疗的所有试验纳入分析,提炼各研究中的中位PFS、发表时间、样本大小、人群特征(如既往内分泌治疗暴露和内脏转移等)等数据,通过线性相关来评估PFS的时间演变趋势。
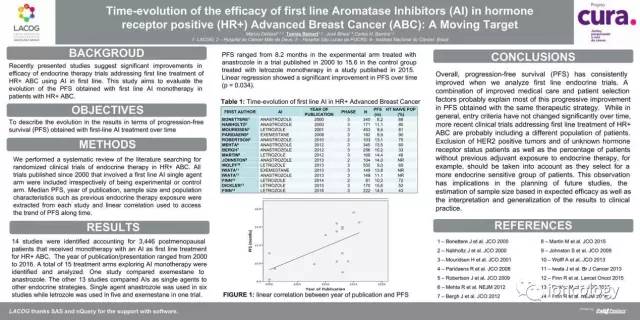
结果确定了13项研究共3446例接受AI单药一线治疗的绝经后HR+ABC患者(研究特征见表1)。研究发表/报告的时间从2000年到2016年。一项研究比较了依西美坦和阿那曲唑,另外12项研究比较了AI和其他内分泌治疗策略。6项研究使用了阿那曲唑单药,5项使用了来曲唑单药,1项使用了依西美坦。2000年到2016年,PFS范围从8.2个月到15.6个月,前者来自2000年发表的研究中使用阿那曲唑治疗的试验臂,后者来自2015年发表的研究中使用来曲唑单药治疗的对照组。线性回归分析显示,随时间发展,PFS得到了显著改善(P=0.034)。
.jpg)
表1. 研究特征
研究者认为:治疗策略相同但PFS逐渐改善,其中的缘由通过医疗护理的改善和患者的选择因素也许能大部分得到解释。尽管一般而言,研究的入组标准并不会随时间变化发生显著改变,但现在的临床试验很可能纳入了和过去不一样的患者群体。例如,除外HER-2阳性肿瘤和HR状态未知的患者,还有既往不曾暴露于内分泌治疗的患者比例也需要考虑——这样就会选择出更多的内分泌治疗敏感的患者。这项研究的结果可对未来试验的设计、样本量的估计(根据预估疗效)以及试验结果的解读和在临床实践中的广泛应用提供一些启示。
原文链接:Debiasi M, Reinert T, Bines J, [P2-08-10]Time-evolution of the efficacy of first line aromatase inhibitors (AI) in hormone receptor positive (HR+) advanced breast cancer (ABC): A moving target. SABCS 2016
附原文
[P2-08-10]Time-evolution of the efficacy of first line aromatase inhibitors (AI) in hormone receptor positive (HR+) advanced breast cancer (ABC): A moving target
Debiasi M, Reinert T, Bines J, Barrios C LACOG - Latin America Cooperative Oncology Group, Porto Alegre, RS, Brazil; Hospital do Cancer Mae de Deus, Porto Alegre, RS, Brazil; Instituto Nacional de Cancer, Rio de Janeiro, RJ, Brazil; PUCRS School of Medicine, Porto Alegre, RS, Brazil
INTRODUCTION. Recently presented studies suggest significant improvements in efficacy of endocrine therapy trials addressing HR+ ABC. Overall, progression-free survival (PFS) has consistently improved when we analyze first line endocrine trials. This study aims to evaluate the evolution of the PFS obtained with first line AI monotherapy in patients with HR+ ABC.
METHODS. We performed a systematic review of the literature searching for randomized clinical trials of endocrine therapy in HR+ ABC. All trials published since 2000 that involved a first line AI single agent arm were included. Median PFS, year of publication, sample size and population characteristics such as previous endocrine therapy exposure and presence of visceral metastases were extracted from each study and linear correlation used to access the trend of PFS along time.
RESULTS. 13 studies were identified accounting for 3,446 postmenopausal patients that received monotherapy with an AI as first line treatment for HR+ ABC. The year of publication/presentation ranged from 2000 to 2016. A total of 14 treatment arms exploring AI monotherapy were identified and analyzed. One study compared exemestane to anastrozole. The other 12 studies compared AIs as single agents to other endocrine strategies. Single agent anastrozole was used in six studies while letrozole was used in five and exemestane in one trial. PFS ranged from 8.2 months in the experimental arm treated with anastrozole in a trial published in 2000 to 15.6 in the control group treated with letrozole monotherapy in a study published in 2015. Linear regression showed a significant improvement in PFS over time (p = 0.034).
.jpg)
CONCLUSION. A combination of improved medical care and patient selection factors probably explain most of this progressive improvement in PFS obtained with the same therapeutic strategy. While in general, entry criteria have not changed significantly over time, more recent clinical trials addressing first line treatment of HR+ ABC are probably including a different population of patients. Exclusion of HER2 positive tumors and of unknown hormone receptor status patients as well as the percentage of patients without previous adjuvant exposure to endocrine therapy, for example, should be taken into account as they select for a more endocrine sensitive group of patients. This observation has implications in the planning of future studies, the estimation of sample size based in expected efficacy as well as the interpretation and generalization of the results to clinical practice.





 京公网安备 11010502033352号
京公网安备 11010502033352号